Home / Work / UnitedHealthcare
Transforming the provider experience through data and insights.
At a glance
UnitedHealthcare Insights (UHC Insights) is a hybrid, analytical and strategic dashboard that centralizes and simplifies complex reporting into an experience that delivers actionable insights to drive sound business decisions and positive performance behaviors.
Audience
For initial release, UHC Insights provided experiences that catered to the needs of an external practice administrator, internal provider advocate and internal senior-level leader. As a note for this case study, “health care professional” and “provider” are used interchangeably.
Challenge & opportunity
Developing the right design strategy involved navigating a complex business landscape, guiding stakeholders on design value and overcoming technical and data limitations, all while facing underestimated challenges with a strong drive for innovation and transformation.
My involvement
I led design strategy and execution across four designers and five delivery teams, contributing to product strategy, UX research, service design, information architecture, wireframes, interaction and visual design and a design pattern library, while being an integral partner in the Agile process.
Research and discovery
Foundations to scale
In the fall of 2018, my UX team and I inherited a strategic concept, uncovering roadblocks in UX, UI scalability and processes that hindered the team's full potential through stakeholder discussions and working sessions.
Getting creative with research
Finding the right enterprise research was challenging, so we leveraged provider panels and partnered with a research team to gain insights into our users despite initial access difficulties.
Insights from discovery
Every persona prefers specificity.
Advanced data filters and customization is a must.
Leaders want more than the “Executive Summary.”
Balancing modern aesthetics and usability will be a give and take relationship.
Instilling trust with our data will be an uphill battle, one that no design may overcome.
Planning and ideation
Working in the Agile environment, these phases are always evolving and shifting, as needed.
IA & UX flows
Through open card sorts with subject matter experts and our research partners, we reimagined the information architecture to better match each of our persona’s mental model and position us for scalability in the future.
Sketching & wireflows
Next, the focus turned to building an infrastructure that prioritized content, implemented dashboard best practices and brought the IA to life with lo-fidelity iterations and wireframe designs.
UI Research
Many hours were also spent exploring usability of data visualization, inspiration for reusable patterns, aligning to a grid system, accessibility and engaging interactions that could make for a delightful brand experience.
Testing and analysis
Embedding a user-centered approach with frequent user touchpoints helped validate and challenge many assumptions.
Active color story with accessibility test of a person with red-green color blindness.
Color surveys
We tested a variety of combinations with user surveys and general opinions that would meet both brand and accessibility requirements. The color story above is the active and primary palette used in the UI today.
For privacy purposes, this is a placeholder graphic to illustrate the report we received.
Nomenclature study
Our language study taught us that while users love specificity, they often struggle with industry jargon. We took these insights into consideration when revising our navigation labels and metric titles.
A typical snippet of a comprehensive usability report from a research partner at Optum Labs
User testing
While scoring some of the highest NPS in the organization, we integrated both full-scale studies and small-scale intercepts, that became enhancement drivers made to data visualization, discoverability, search and navigation.
Execution of final interface
Below are a few key-pages designed & built for our external persona and what we know today as UnitedHealthcare Insights (UHC Insights).
Storytelling by the numbers
There are two things providers care about most: delivering the highest quality of care to their patients and getting paid for it. Taking that into account, we built an overview that focuses on reimbursements with secondary reporting on care management and operational efficiency.
(Our internal dashboards—while not shown in the case study—focus on provider performance as well as internal reporting of satisfaction surveys and larger geographical data, resulting in unique views for each persona.)
A “slice and dice” kind of user
The goal of each workflow was to surface significant data points through progressive drill-downs, interactive data visualizations and advanced filtering. Our users like specificity and they certainly get it with UHC Insights.
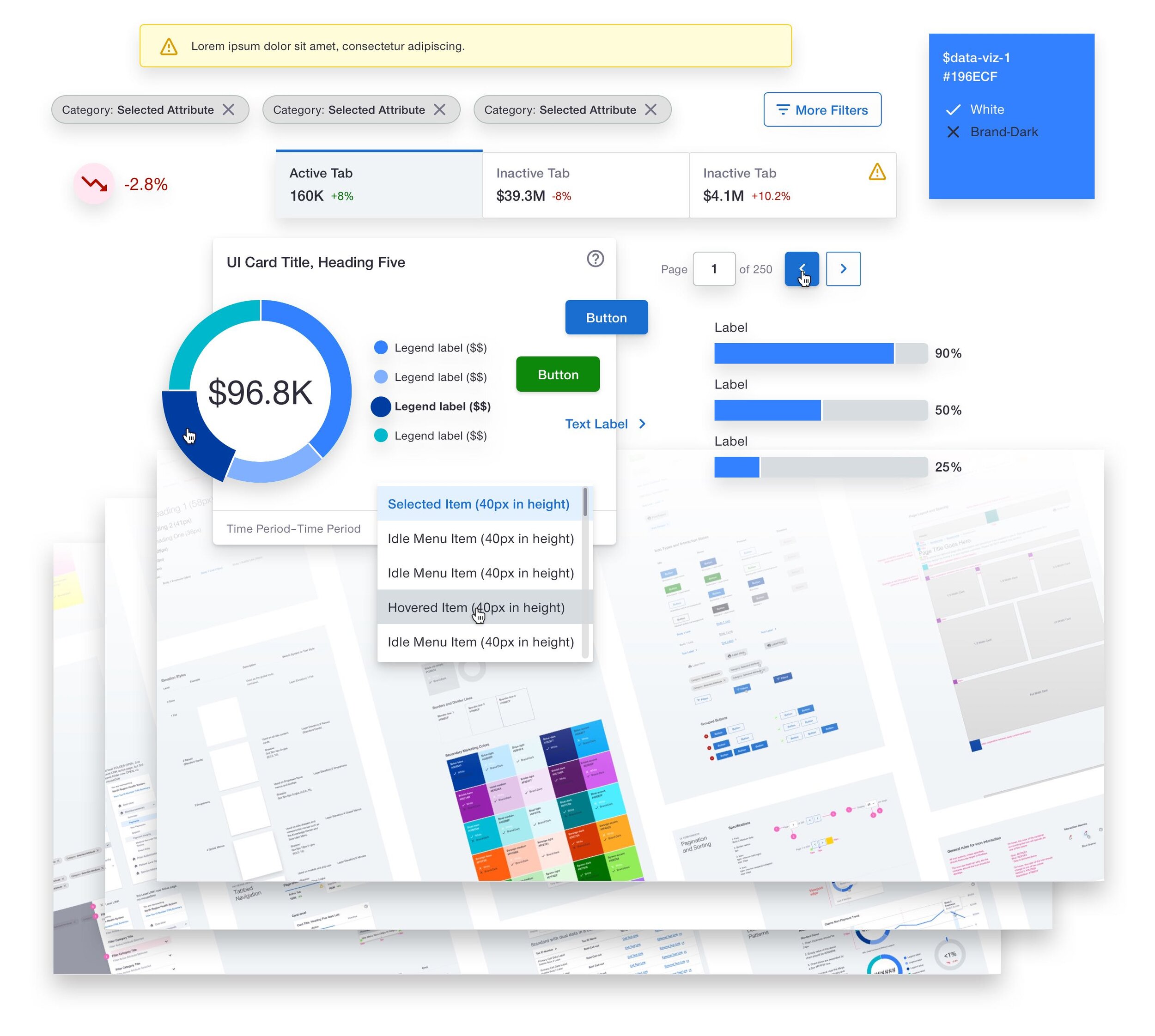
Data filtering & user support through common UX
We took many patterns found in the everyday retail setting and productivity tools to increase recognition, usability and provide immediate value.
Design for scale & consistency
From inception to strategy and execution, I led the team through the creation of a design pattern library to increase efficiency in our process as well as in the implementation phase with reusable web components.
Staying consistent as a designer-of-one is never an easy task, let alone four others. This library of foundational brand, components, patterns and templates was integral in driving consistency and quality towards the brand promise delivered.
Takeaways & lessons learned
After a year of piloting, UHC Insights went live to all external health care systems in the network as well as many internal business teams in late 2019 and early 2020.
Though I was faced with many tough decisions, challenging conversations, frequent hiccups in the data and roadmap pivots, UHC Insights has become a new standard of innovation for the organization. It will continue to serve as a tool of transparency where payer and provider can meet together, to take action on opportunities that lower the total cost of care to the UnitedHealthcare network and its members.